AI Workers’ Comp Claims Agent
Automating Claims Processing with AI
Jurisdiction-Aware Intake and EDI Filing
AI automation captures claim data from any channel—portals, calls, email, or fax—validates coverage, classifies the event, and files FROI/SROI transactions per IAIABC R3.1 specifications with automatic error handling and resubmission.
Predictive Triage and Reserve Accuracy
Risk scoring models evaluate body part, injury mechanism, jurisdiction, comorbidities, and attorney involvement likelihood on day one, routing claims to the right skill level and flagging reserve mismatches before they become leakage.
Automated Bill Review and Payment
Medical bills are ingested, normalized, repriced against state fee schedules and PPO contracts, audited for upcoding and unbundling, and processed through UR workflows—accelerating payment cycles while controlling medical spend.
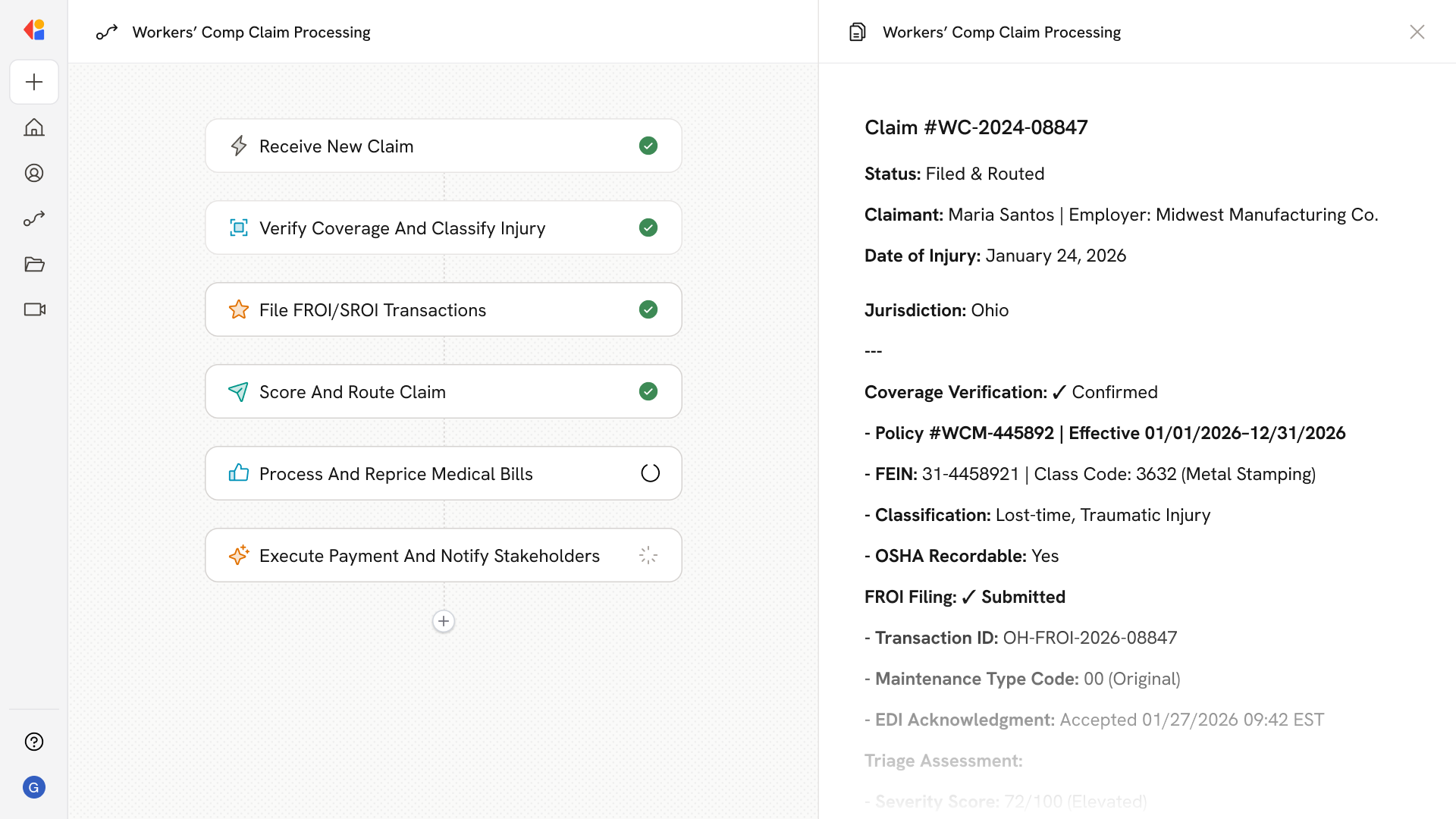
How Cassidy automates workers' comp claims using AI
Step 1: Trigger on new claim intake
The Workflow activates when a new workers' comp claim arrives—whether from an employer portal, HR submission, call center, email, fax, or EDI feed. Cassidy parses structured and unstructured data using OCR and NLP to capture injury details, employer information, and supporting documentation.
Step 2: Verify coverage and classify the event
Cassidy pulls policy data, validates employer FEIN and class codes, confirms insured status, and classifies the event as traumatic vs. occupational disease, medical-only vs. lost-time, and determines OSHA recordability—populating the required DN fields for the applicable jurisdiction.
Step 3: Generate and file FROI/SROI transactions
Based on jurisdiction rules and IAIABC R3.1 specifications, Cassidy creates the appropriate FROI or SROI transaction with the correct Maintenance Type Code, submits via secure file transfer, monitors acknowledgments, and automatically corrects and resubmits rejected filings.
Step 4: Triage and route the claim
Cassidy's predictive models score the claim for severity, attorney involvement risk, and reserve adequacy on day one. Claims are routed to the appropriate team—medical-only, lost-time, or complex/litigated—with action plans, diaries, and escalation flags set automatically.
Step 5: Process medical bills and UR workflows
Incoming bills are ingested, normalized, deduplicated, and repriced against state fee schedules and network contracts. Cassidy applies clinical edits, flags specialty audits, runs utilization review against ODG/ACOEM guidelines, and generates determination letters—all with Human-in-the-Loop approval for complex decisions.
Step 6: Execute payment and update stakeholders
Approved bills trigger EOB generation, lien and withholding calculations, and electronic payment. Cassidy sends statutory notifications, updates SROI filings for benefit changes, and keeps adjusters informed with consolidated dashboards—so they stay focused on investigation, RTW coordination, and claimant communication.
Implement it inside your company
- Hands-on onboarding and support
- Self-paced training for your team
- Dedicated implementation experts
- Ongoing use case discovery
- ROI tracking & analytics dashboards
- Proven playbooks to get started fast