AI Claims Triage Agent
Automating Claims Triage with AI
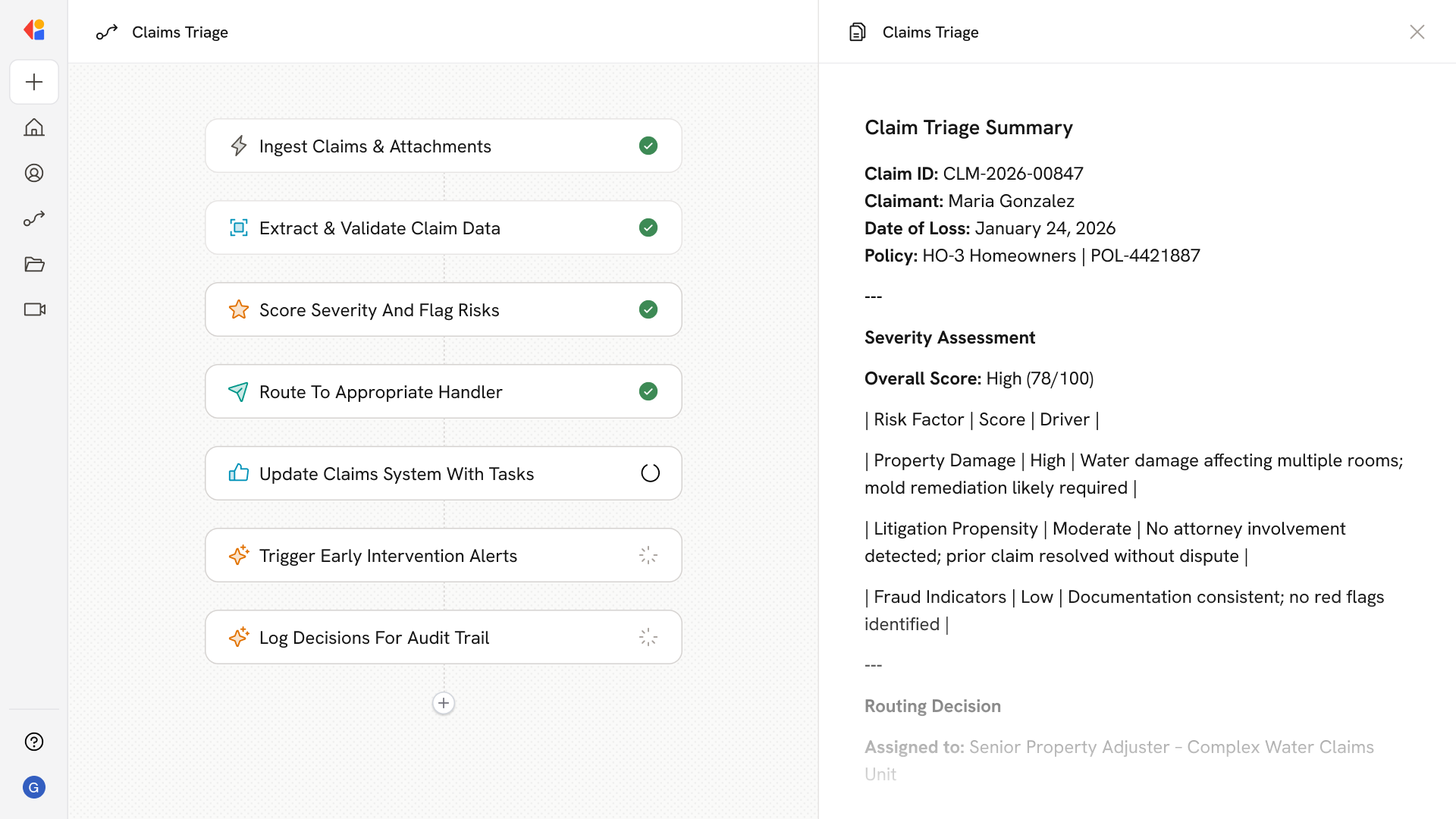
Explainable Risk Signals That Adjusters Trust
Every claim receives a severity and complexity score backed by rank-ordered drivers—attorney involvement, surgical indicators, pharmacy triggers—so adjusters understand exactly why a claim was flagged and can act with confidence.
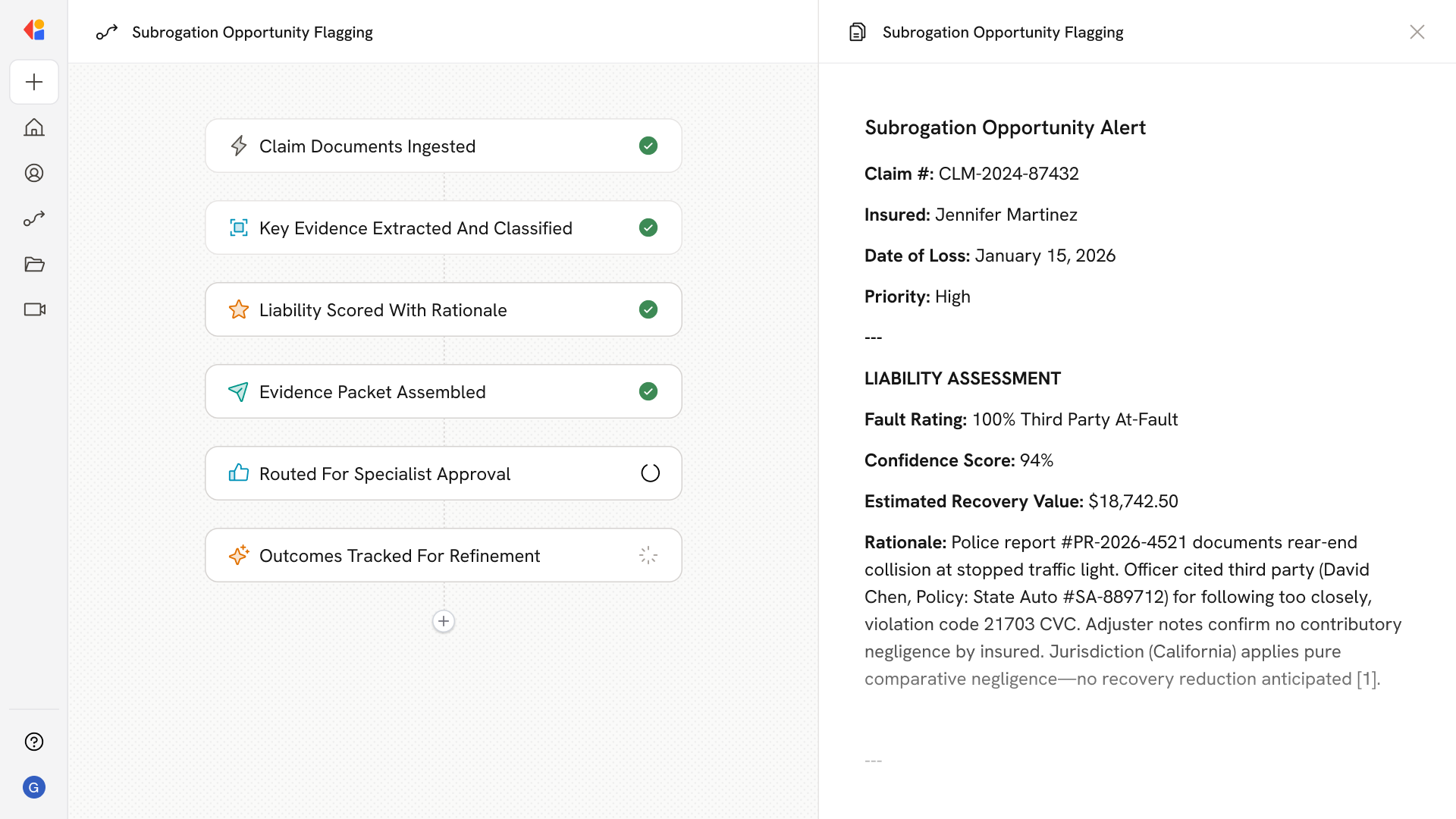
Routing Rubrics That Match Claims to the Right Path
Business rules automatically map risk scores and claim attributes to handling queues—fast-track, standard, complex, SIU, litigation, or nurse case management—balancing workloads and enforcing SLA timelines without manual sorting.
Early Interventions That Prevent Severity Escalation
Real-time alerts surface claims showing cost spikes, new litigation signals, or medical management needs, enabling targeted actions before innocuous-looking claims turn into high-cost exposures.
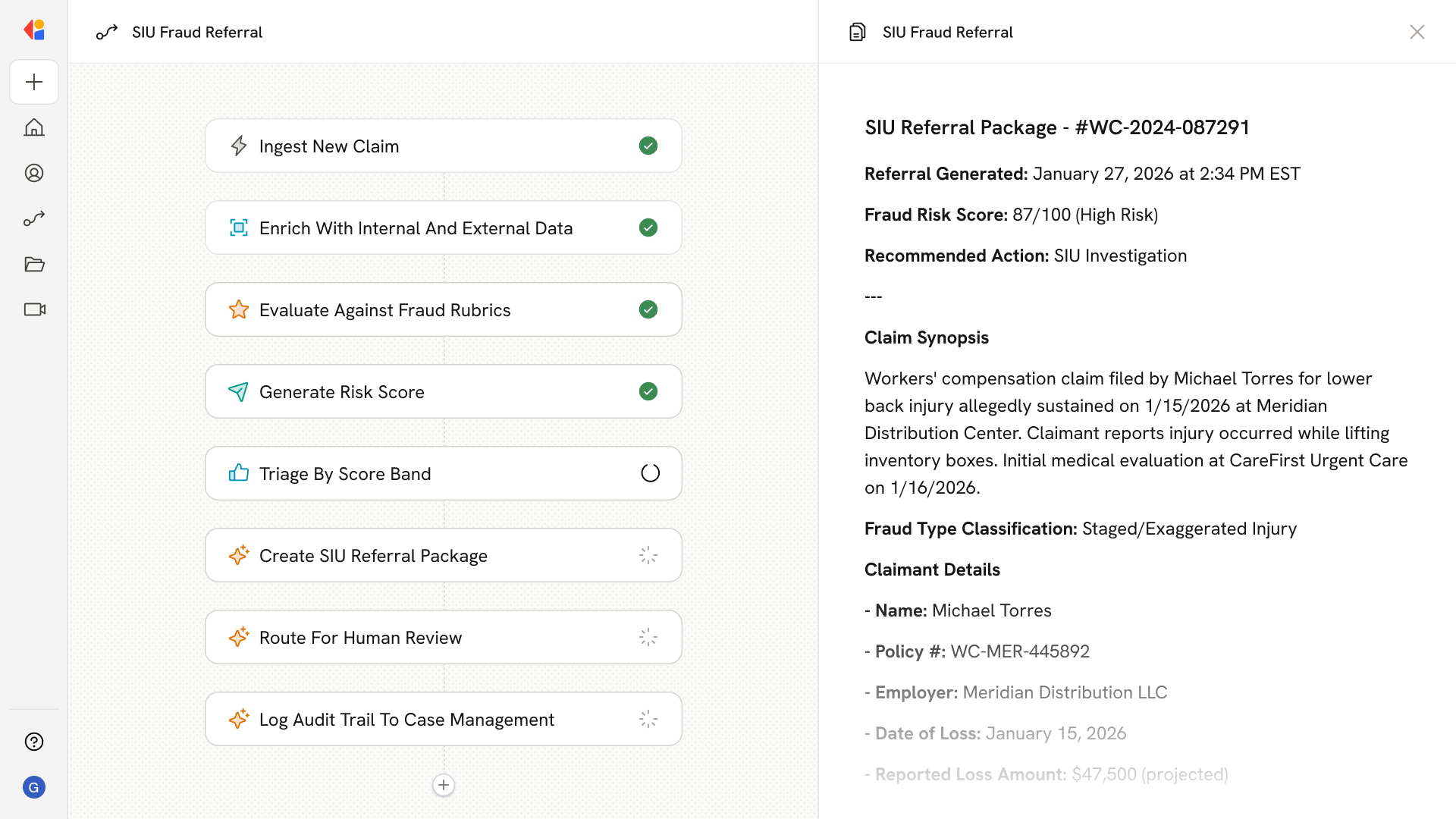
How Cassidy automates Claims Triage using AI
Step 1: Ingest FNOL and claim artifacts
The Workflow triggers when a new claim arrives—via portal submission, email, call center entry, or broker upload—and pulls in attachments like photos, police reports, medical bills, and ACORD forms.
Step 2: Extract and normalize claim data
Cassidy reads unstructured documents using OCR and AI extraction, identifying claimant details, loss descriptions, injury types, parties involved, and coverage information, then validates against policy data in your core system.
Step 3: Score severity and flag risk signals
The Workflow runs the claim through your risk models to generate severity, litigation propensity, and fraud scores, surfacing explainable drivers—such as "opioid Rx filled," "attorney keyword detected," or "prior claims history"—as risk notes for adjusters.
Step 4: Apply routing rubrics and assign
Cassidy executes your business rules to determine the handling path: fast-track for low-complexity claims, SIU referral for fraud flags, nurse triage for Workers' Comp surgical indicators, or senior adjuster assignment for high-exposure cases.
Step 5: Update claims system and set tasks
The Workflow writes back to Guidewire, Duck Creek, or your claims management system—creating the claim file, setting initial reserves aligned to predicted severity, assigning tasks and diary entries, and notifying the appropriate team.
Step 6: Trigger early interventions and alerts
As new information arrives, Cassidy continuously rescores the claim and sends real-time alerts when severity changes, an attorney is retained, or medical management is needed—enabling proactive action before costs escalate.
Step 7: Document rationale for audit and compliance
Every triage decision is logged with citations back to source documents, creating a complete audit trail that supports regulatory reviews and enables performance benchmarking against LAE and cycle-time targets.
Implement it inside your company
- Hands-on onboarding and support
- Self-paced training for your team
- Dedicated implementation experts
- Ongoing use case discovery
- ROI tracking & analytics dashboards
- Proven playbooks to get started fast