AI Adjuster Notes Summarization Agent
Automating Adjuster Notes Summarization with AI
Cut through thousands of pages in minutes
The Agent processes claim notes, emails, medical records, and litigation documents, converting scattered updates into a single, decision-ready brief.
Deliver consistent, category-aligned summaries
Automated Workflows produce standardized outputs across coverage, medical, financial, and litigation categories—so every claim review follows the same structure.
Keep adjusters in control with traceable citations
Every summary statement links back to its source document and page, giving your team the auditability they need for internal reviews and regulatory scrutiny.
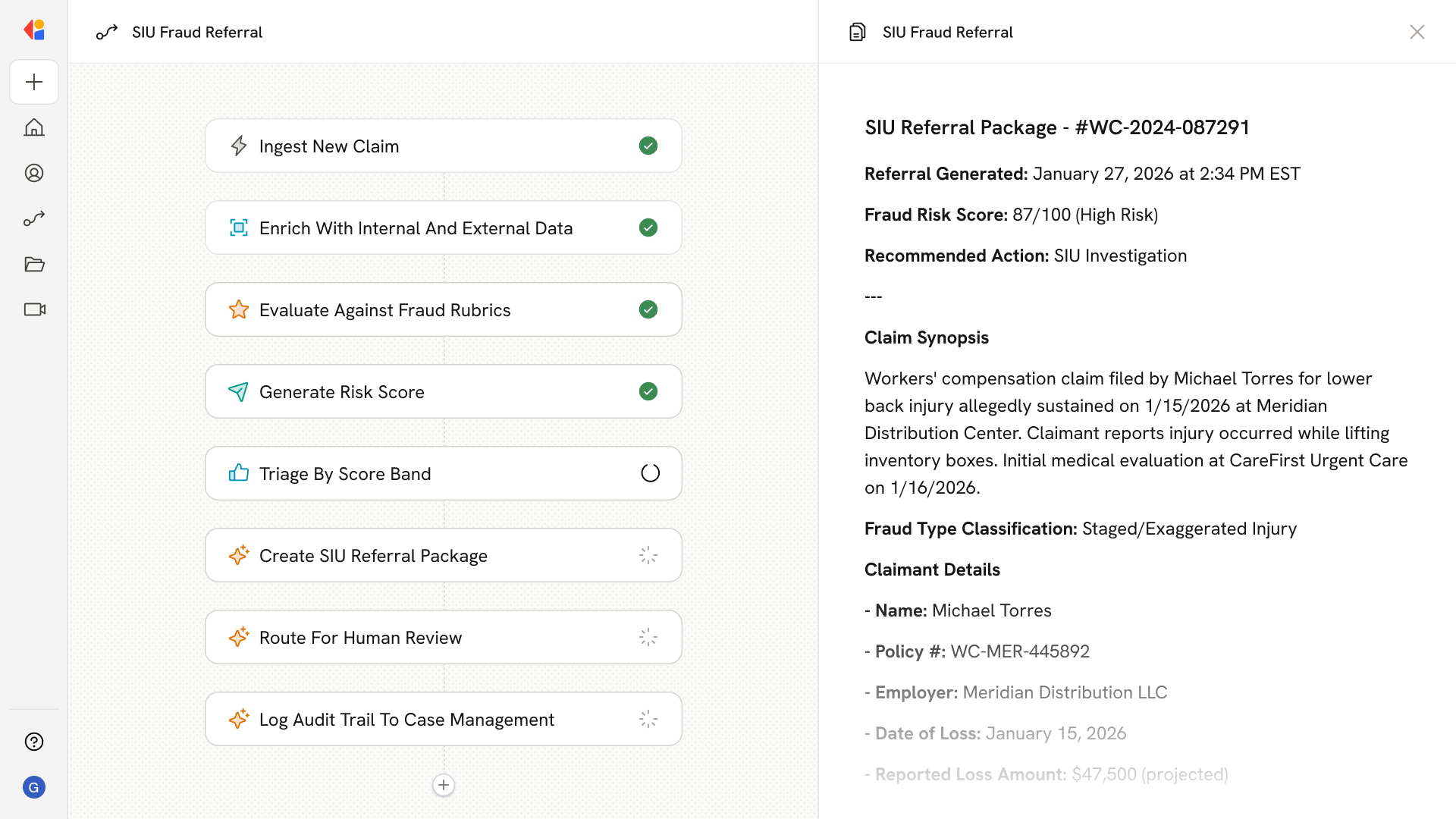
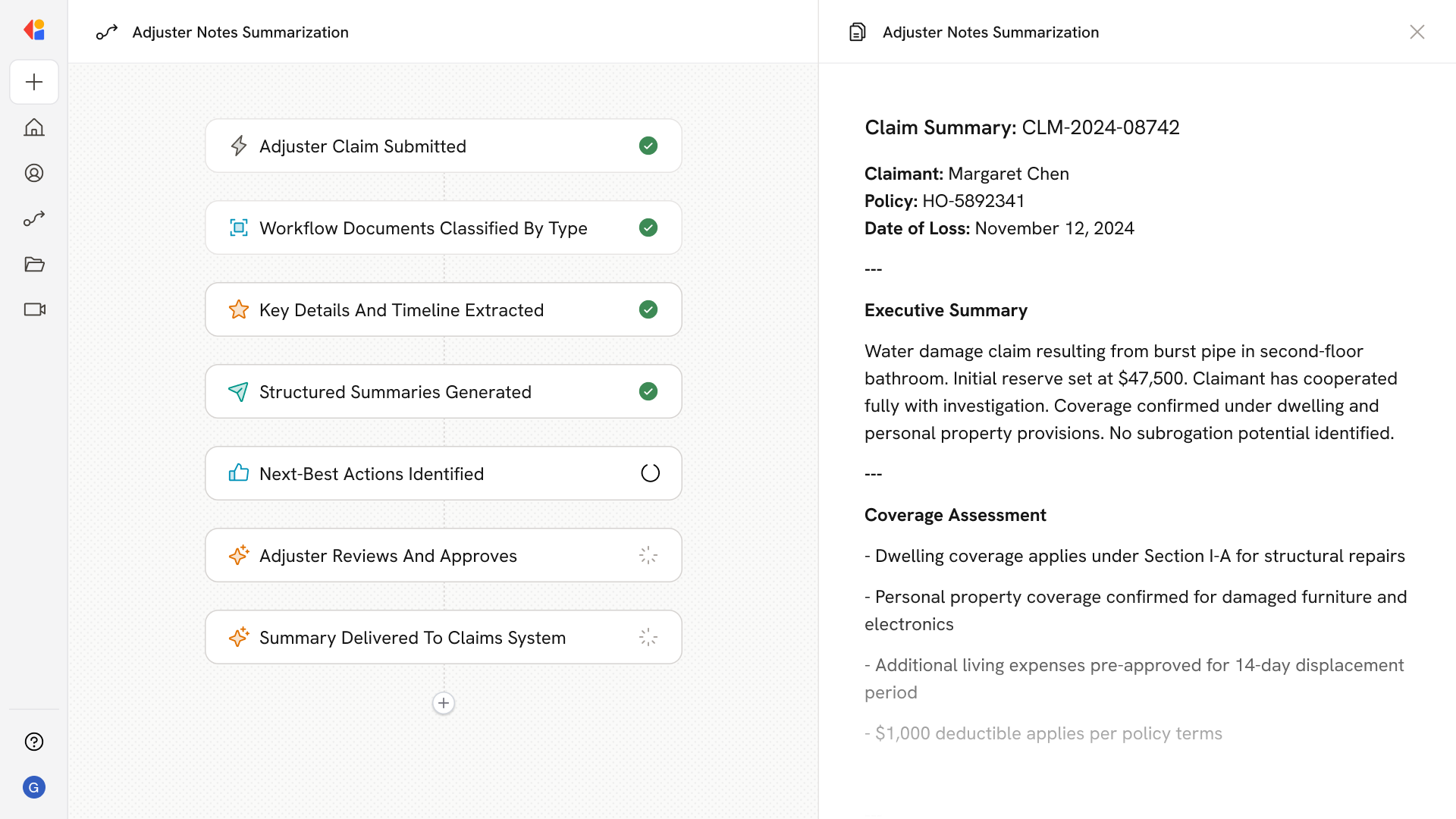
How Cassidy automates adjuster notes summarization using AI
Step 1: Trigger on new or updated claim
The Workflow activates when a claim is created or updated in your claims management system, or when new adjuster notes, medical records, or litigation documents are added.
Step 2: Ingest and classify documents
Cassidy pulls claim notes, emails, PDFs, and scanned files from connected sources, classifying each by type—adjuster note, medical report, legal filing, repair estimate—and normalizing dates, parties, and policy identifiers.
Step 3: Extract entities and build timelines
The Agent extracts key details: coverage terms, claimant information, loss dates, provider names, ICD/CPT codes, reserves, payments, and litigation milestones. It reconstructs a chronological timeline from FNOL through resolution.
Step 4: Generate structured summaries
Cassidy produces an executive brief and category-specific summaries—coverage stance, medical chronology, financials, litigation status, and pending actions—with each statement linked to its source for full traceability.
Step 5: Surface next-best actions
The Workflow identifies follow-ups: missing records to request, IME scheduling, negotiation windows, court deadlines, and reserve adjustments—delivered as a prioritized action list.
Step 6: Human-in-the-Loop review
Before delivery, summaries route to a claims professional for validation. Adjusters can correct inaccuracies, confirm completeness, and approve the final output.
Step 7: Deliver to claim systems and worklists
Approved summaries push directly into your CMS, RMIS, or adjuster dashboard—ready for review packets, QC audits, or conversational Q&A over claim history.
Implement it inside your company
- Hands-on onboarding and support
- Self-paced training for your team
- Dedicated implementation experts
- Ongoing use case discovery
- ROI tracking & analytics dashboards
- Proven playbooks to get started fast