AI Medical Bill Review Agent
Automating Medical Bill Review with AI
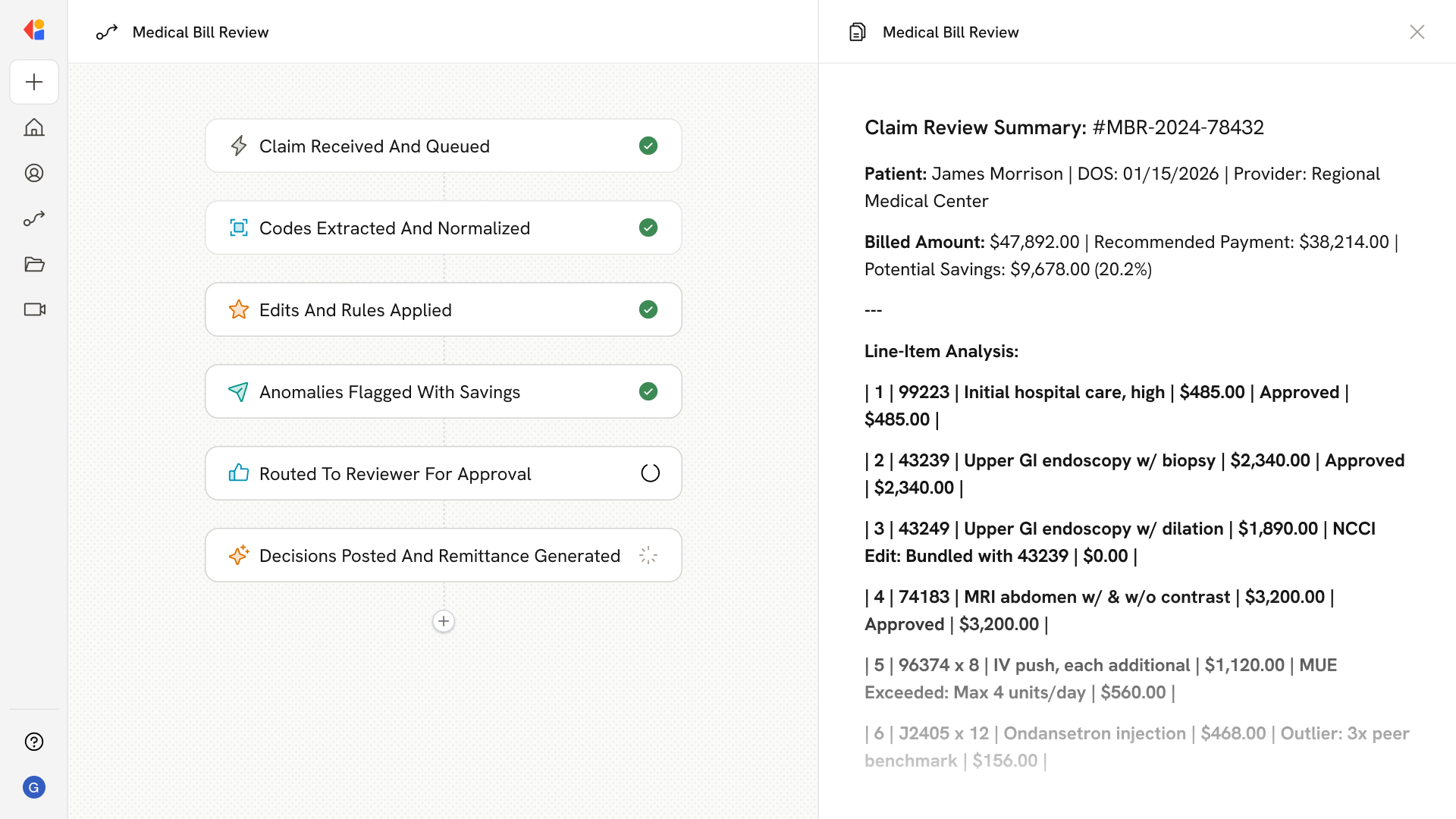
Extract and validate coded data automatically
The Agent ingests claims via EDI 837, PDF bills, and itemized charges, then uses OCR and NLP to extract ICD-10, CPT/HCPCS codes, modifiers, and service details into structured, normalized records.
Flag anomalies and apply payment integrity rules
Automated edits—including NCCI PTP, MUE, OCE, and DRG validation—catch upcoding, unbundling, duplicate billing, and modifier misuse, with each flag tied to a specific rule citation or statistical rationale.
Route complex claims to reviewers with full context
High-risk or high-dollar claims surface in prioritized worklists, giving nurse auditors and coding specialists the AI recommendation, supporting documentation, and rule references they need to confirm, override, or escalate.
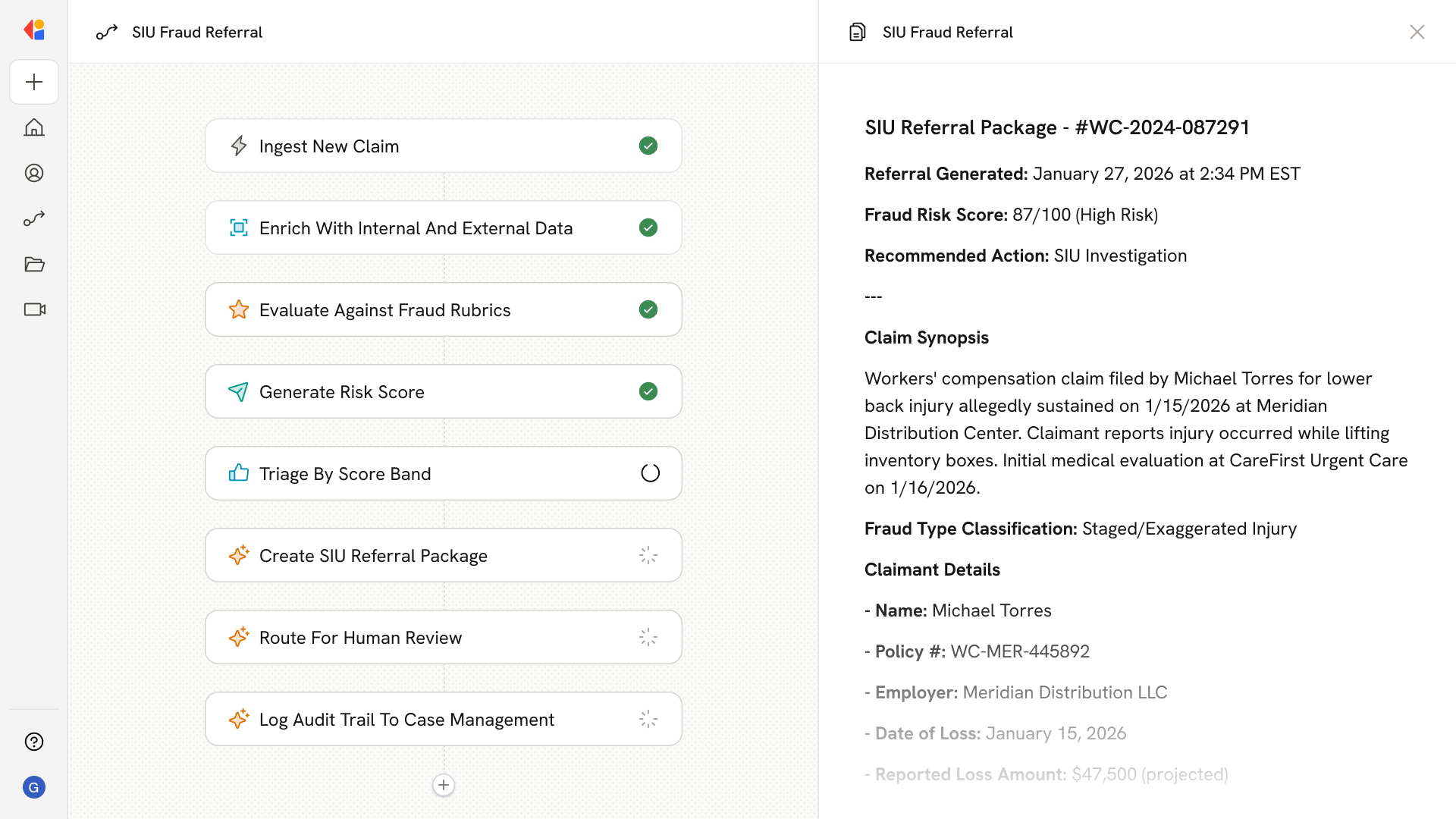
How Cassidy automates Medical Bill Review using AI
Step 1: Trigger on new claim or bill submission
The Workflow activates when a claim arrives—whether via EDI 837 feed, scanned PDF (CMS-1500, UB-04), or clearinghouse upload—and queues it for processing.
Step 2: Extract and normalize coded data
Cassidy parses line items, diagnosis codes (ICD-10-CM/PCS), procedure codes (CPT/HCPCS), modifiers, units, service dates, and provider identifiers, mapping everything to your internal claim schema.
Step 3: Run coding edits and payment rules
The Workflow applies NCCI PTP and MUE edits, OCE/OPPS logic, DRG grouper validation, and your payer-specific fee schedules—flagging incompatible code pairs, excessive units, and pricing variances.
Step 4: Detect anomalies and calculate savings
Cassidy's analytics identify upcoding, unbundling, duplicate charges, and outlier patterns, then compute line-level and claim-level savings with transparent rationale and peer benchmarks.
Step 5: Route to reviewer with Human-in-the-Loop
Claims that exceed risk or dollar thresholds land in prioritized worklists. Reviewers see the AI recommendation, supporting medical records, rule citations, and confidence scores—then confirm, adjust, or escalate.
Step 6: Post adjudication decisions and generate remittance
Once approved, Cassidy pushes determinations back to your core claims system, produces 835 remittance advice with appropriate CARC/RARC codes, and logs every decision for audit and appeals.
Implement it inside your company
- Hands-on onboarding and support
- Self-paced training for your team
- Dedicated implementation experts
- Ongoing use case discovery
- ROI tracking & analytics dashboards
- Proven playbooks to get started fast