AI Auto Damage Claim Triage Agent
Automating Auto Claims Document Triage with AI
Turn messy, multi-channel submissions into claims-ready files
AI automation ingests emails, web forms, PDFs, and photos, then classifies, extracts, and normalizes every data point into a structured claim file with full source citations.
Identify gaps and request missing documentation automatically
The agent runs completeness checks against your SOPs and jurisdiction requirements, then sends targeted requests for missing police reports, scene photos, or authorizations—with SLA tracking and escalation paths built in.
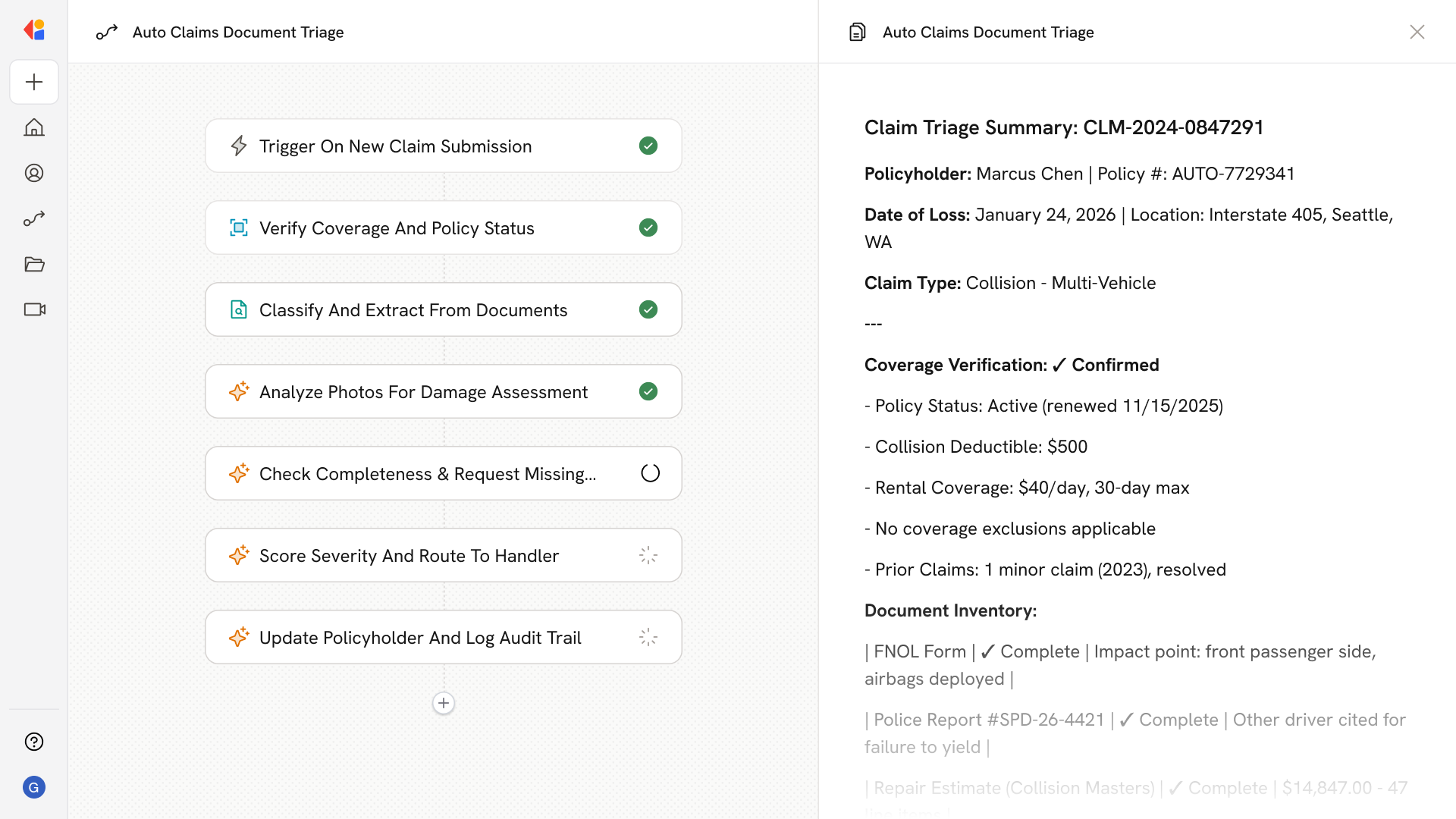
Route claims to the right appraiser with confidence
Severity scoring evaluates damage, coverage complexity, fraud signals, and injury presence to assign claims to desk appraisers, field inspectors, DRP shops, total loss units, or SIU—balancing workload and reducing misrouting.
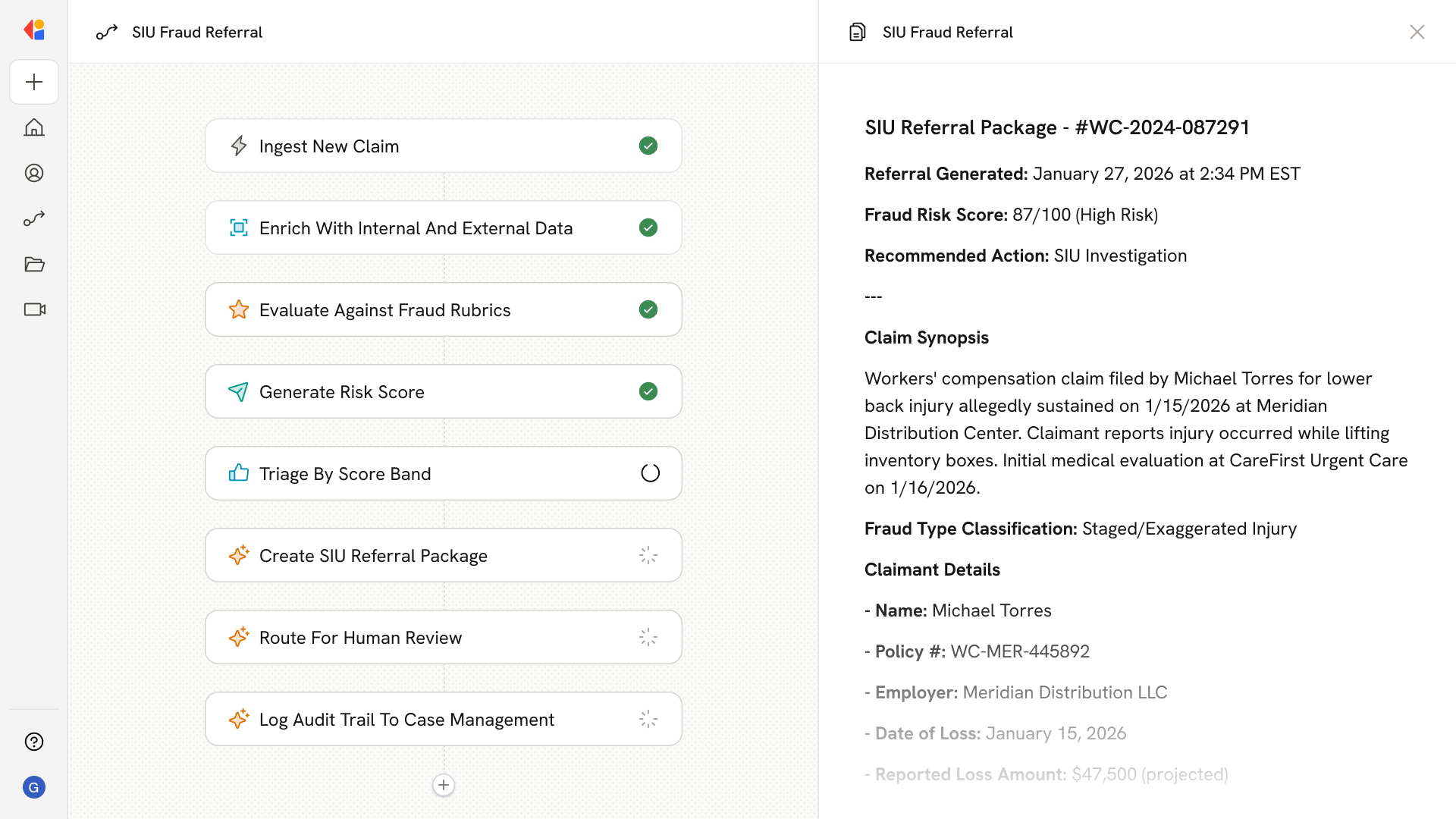
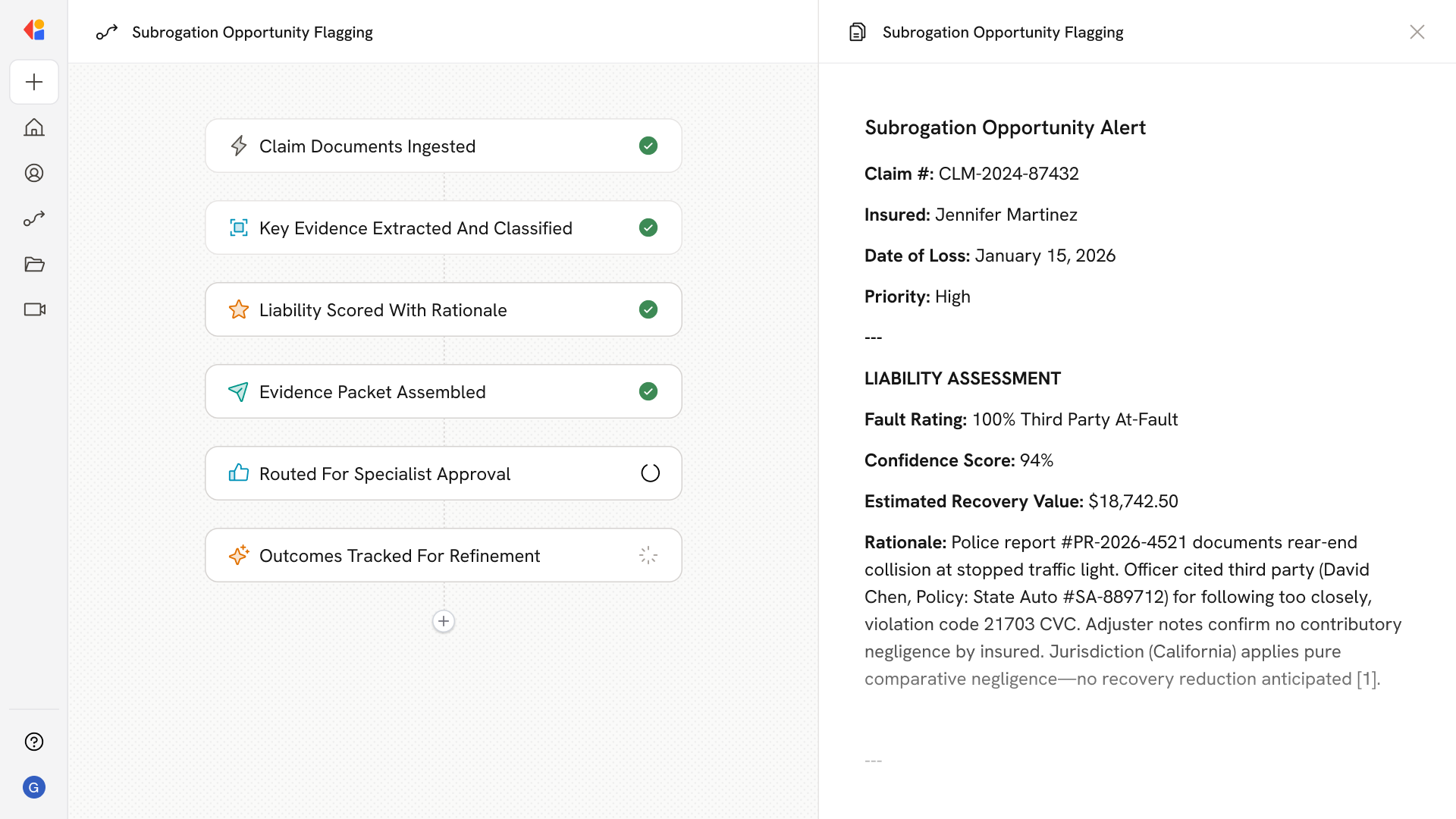
How Cassidy automates auto claims document triage using AI
Step 1: Trigger on new claim submission
The Workflow activates when a new FNOL arrives—whether from email, web portal, mobile app, or broker feed—capturing policyholder details, incident narrative, vehicle information, and initial photos.
Step 2: Verify coverage and policy status
Cassidy pulls policy data from your claims management system to confirm coverage, deductibles, exclusions, and prior claims history, flagging any eligibility issues before triage begins.
Step 3: Classify and extract from all documents
The Workflow processes every attachment—FNOL forms, police reports, repair estimates, invoices, statements—using AI to classify document types and extract key fields into a normalized, claims-ready dataset.
Step 4: Analyze photos and detect damage
Cassidy evaluates submitted photos to identify damaged components, predict repairable vs. total loss scenarios, and generate preliminary line-level estimates for appraiser review.
Step 5: Run completeness checks and request missing items
The agent compares the claim file against your completeness checklist by loss type and jurisdiction, then auto-generates targeted requests via email, SMS, or portal with SLA-tracked reminders.
Step 6: Screen for fraud and anomalies
Cassidy flags inconsistencies—timestamp mismatches, duplicate patterns, suspicious providers, inflated line items—and routes high-risk claims to SIU with documented rationales.
Step 7: Score severity and route to the right handler
Based on damage severity, coverage complexity, liability factors, and fraud risk, the Workflow assigns claims to desk appraisers, field inspectors, DRP shops, total loss units, or casualty adjusters—with Human-in-the-Loop approval for high-stakes decisions.
Step 8: Update status and maintain audit trail
Cassidy sends omnichannel status updates to the policyholder and logs every decision, extraction, and routing action with source citations for compliance and QA.
Implement it inside your company
- Hands-on onboarding and support
- Self-paced training for your team
- Dedicated implementation experts
- Ongoing use case discovery
- ROI tracking & analytics dashboards
- Proven playbooks to get started fast