AI SIU Referral Agent
Automating SIU Referrals with AI
Governed rubrics that codify your red flags
The Agent applies your organization's fraud indicators and regulatory requirements as versioned, policy-based rules that fire with reason codes and evidence pointers.
Risk scoring with explainable reason codes
ML models evaluate each claim for fraud propensity, surfacing the top drivers behind every score so adjusters and SIU teams understand exactly why a claim was flagged.
Audit-ready decision trails from intake to disposition
Every trigger, score, human override, and evidence attachment is logged in an immutable record—ready for regulatory examinations and legal challenges.
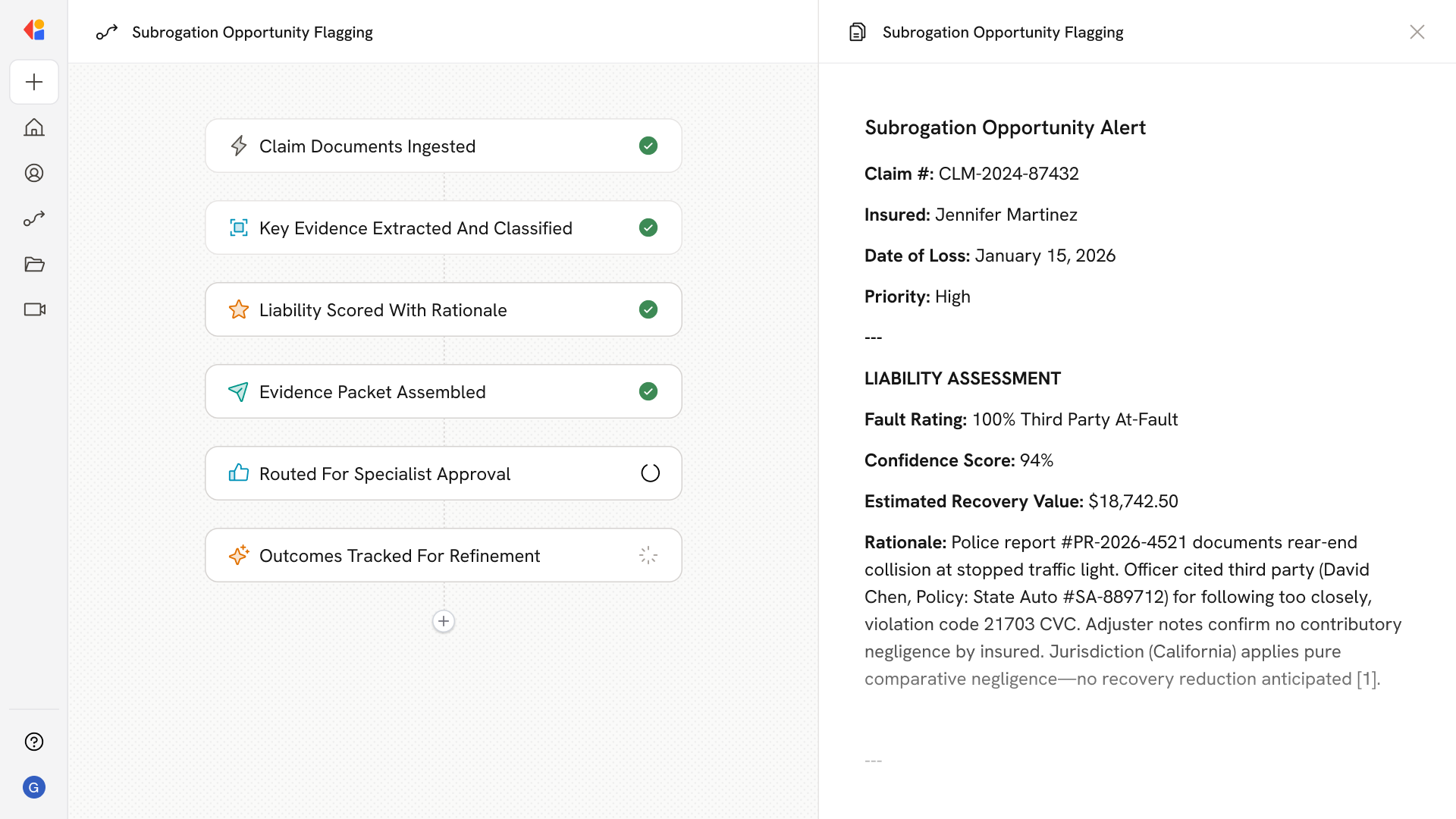
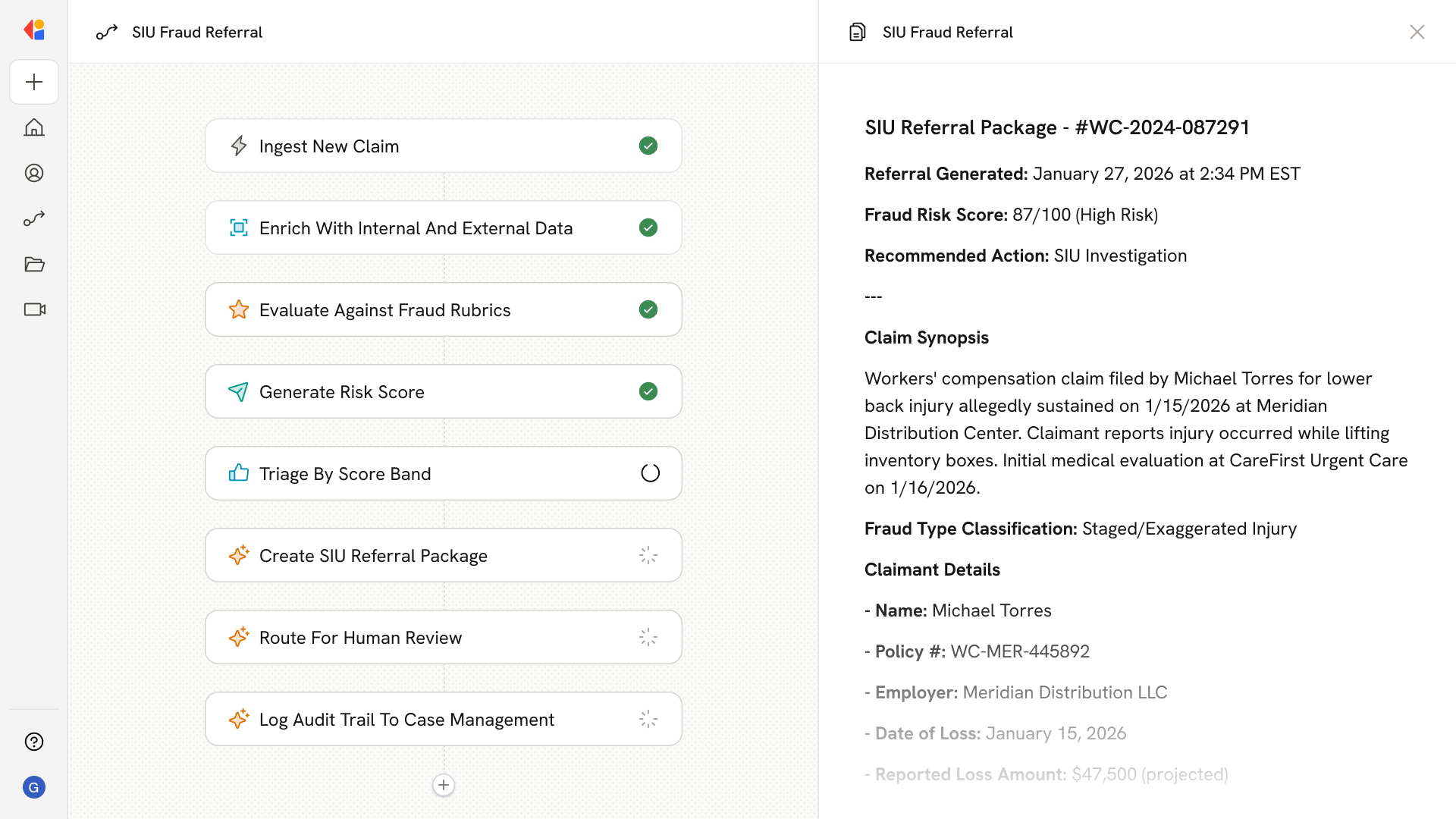
How Cassidy automates SIU Referrals using AI
Step 1: Trigger on new claim or FNOL event
The Workflow activates when a new claim enters your system—whether from a portal submission, contact center intake, or TPA feed—pulling in policy details, coverage status, and loss information.
Step 2: Enrich with internal and external data
Cassidy pulls claims history, prior losses, SIU records, and policy data from your systems, then enriches with consortium sources like ISO ClaimSearch, public records, and provider databases to build a complete picture.
Step 3: Apply governed fraud rubrics
The Agent evaluates the claim against your codified red-flag catalog—LOB-specific indicators, regulatory definitions, and watchlists—firing rules that produce reason codes and link directly to supporting evidence.
Step 4: Generate risk score with reason codes
Cassidy scores the claim for fraud propensity using ML models, returning a risk score alongside the top drivers so your team sees exactly what triggered the flag.
Step 5: Triage and route by score band
Claims are segmented into work queues based on score thresholds: low-risk claims fast-track to processing, amber claims route to adjuster review, and high-risk claims escalate toward SIU referral.
Step 6: Generate SIU referral package
When “reasonable belief” thresholds are met, Cassidy auto-generates a referral package with synopsis, fraud type, party details, amounts, reason codes, and evidence attachments—formatted to meet state regulatory requirements.
Step 7: Human-in-the-Loop review and routing
Adjusters or SIU leads review the referral, with the ability to approve, suppress, or escalate—each action logged with documented justification that feeds back into model improvement.
Step 8: Log audit trail and sync to case management
Cassidy writes the complete decision trail—data sources, triggers fired, scores, human actions, and timestamps—to your case management system, ready for regulatory examination or legal review.
Implement it inside your company
- Hands-on onboarding and support
- Self-paced training for your team
- Dedicated implementation experts
- Ongoing use case discovery
- ROI tracking & analytics dashboards
- Proven playbooks to get started fast